Deborah Copaken anxiously felt the prick of the needle in her arm under the stark lights of the hospital room as she prepared to be sedated.
The Brooklyn-based mother-of-three was about to undergo a vital operation to help her hear again after the sudden onset of deafness from a COVID infection in the summer of 2022.
Her doctor, Dr. Babak Sadoughi, was already scrubbed and ready for surgery.
But then, just seconds before she was set to be wheeled into the operating room, her insurance company – UnitedHealthcare – contacted the doctor’s office.
Approval for the procedure had been denied as it was ‘not medically necessary’.
Copaken, 58, shared her traumatic experience with DailyMail.com in the wake of the cold-blooded assassination of UnitedHealthcare CEO Brian Thompson, 50.
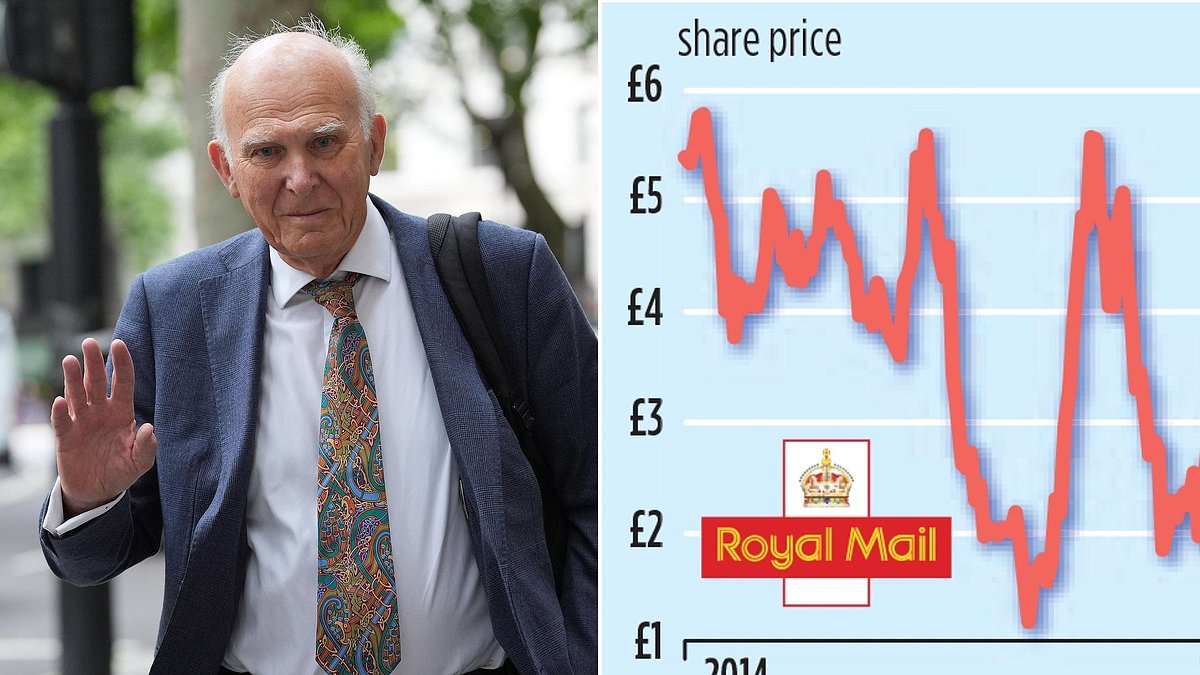
Thompson was fatally shot on the street outside the New York Hilton Midtown in Manhattan, New York City on December 4.
His alleged killer, privately educated former Ivy League student Luigi Mangione, 26, scion of a prominent Maryland family, was arrested on December 9 at a McDonald’s restaurant in Altoona, Pennsylvania.
Thompson’s murder sparked a spontaneous wave of people sharing their ire on social media about being denied approval for operations by United, the nation’s largest health insurance company.

UnitedHealthcare denied Deborah Copaken coverage just two minutes before her surgery was scheduled to begin, claiming ‘this procedure is not medically necessary for you’

Three shell casings found at the scene had ‘deny’, ‘depose’ and ‘defend’ etched into them, hinting that the motive could be related to UnitedHealthcare’s business practices

UnitedHealthcare boss Brian Thompson was gunned down outside the Hilton Hotel in Midtown Manhattan on December 4 in what police said was a targeted attack
When the company denied Copaken’s claim, she claimed her doctor told her, ‘I’m so sorry. They’re doing this on purpose. I deal with this stuff every day.’
And, as the line for the anesthesia was removed from Copaken’s arm, the attending nurse commented, ‘I’ve seen them deny care before but never like this.’
Crushed, in tears, and still unable to hear, she was sent home to suffer in continued, unnecessary silence.
Speaking to DailyMail.com, Copaken said: ‘The nature of the denial, given that I was already in a hospital gown and ready for surgery, felt blatantly evil, deliberate in its timing, and wrong.
‘I felt totally hopeless. It really clobbered me, hard – it was a final straw moment. United was sentencing me to a life of discomfort, pain, and silence which I ended up enduring for more than a year.’
‘God knows how much better my hearing would be now had I been able to get that operation back then,’ she continued.
An acclaimed photographer and author who has written extensively about the ‘dangers and absurdities of for-profit healthcare,’ Copaken had spent weeks communicating with United about needing treatment to save her hearing.
She writes about her experience with United on her Substack page, ‘Ladyparts,’ and has penned a bestselling book with the same title about the healthcare industry.
‘I went deaf from the inflammation that shut down my Eustachian tubes and essentially glued them shut with scar tissue. In the wake of that, I did everything by the book,’ she told DailyMail.com.
‘This was a clear-cut case of medical need. From one day to the next, in the summer of 2022, I went deaf from Covid.’
Steroids didn’t work and Dr Sadoughi tried a balloon Eustachian tube dilation surgery under local anesthesia.
‘It was so excruciatingly painful, because I have a deviated septum, that I screamed throughout the entire procedure, and we had to abandon it,’ Copaken shared on her Substack the day after Thompson’s murder.
‘Next, we planned my surgery under general anesthesia. United required pre-authorization, so we planned the operation several weeks in the future to leave time for that. United kept delaying getting back to my surgeon.
‘They essentially went radio silent for weeks. I got some hearing aids at Costco, just so I could hear my kids and other humans in the meantime.’
Despite her doctor’s office calling United every day, by the day of the surgery there was still no word about whether the $40,000 procedure would be covered.
‘So we just acted as if this absolutely necessary and critical surgery would be covered. Because why would it ever not be?’ she explained.
Her doctor recommended that she write to United appealing the last-minute denial and explaining why the operation was so crucial. But the company refused to back down.
She was sent a second and final denial which said: ‘Based on review of this case balloon dilation has not been shown to be an effective treatment for stopped up ears. This service is not covered. The studies are in small numbers of patients.’
The procedure was eventually approved in October 2023 by Copaken’s new insurance company, Fidelis, which – without any denials – deemed the procedure ‘medically necessary.’
She told DailyMail.com: ‘I had immediate relief following the surgery. I’d lived with closed Eustachian tubes for over a year. It was insane and painful and it made it impossible to hear or travel or feel comfortable.’
And she noted on her Substack, ‘For those of us unlucky enough to nearly die or go deaf or get sick, or if you’re me, all three and more, dealing with our American healthcare system…can and often does feel like going up against the mafia, again and again, only to get kneecapped and go bankrupt every goddamned time.
‘My hearing is still impaired, but it’s at least clearer than it was pre-surgery. Of course, I’ll never know how much clearer it could have been, had United not kicked me out of the hospital, minutes before my first surgery was set to begin.’
She added that she is ‘shocked and horrified’ by the murder of Thompson. She also decries the ‘health insurance greed’ and calls UnitedHealthcare Group the ‘worst of the worst.’
‘Perhaps this murder, sad as it is for Thompson’s family and friends…can serve as a wakeup call. Americans are tired of fighting to stay alive. We’re tired of hearing that healthcare is a privilege and not the basic human right every other country deems it to be,’ she wrote on Substack.

Copaken’s op-ed also detailed how her three pregnancies cost her $27,000 out of pocket, despite being on a high-end UnitedHealthcare plan, and other battles with the insurer

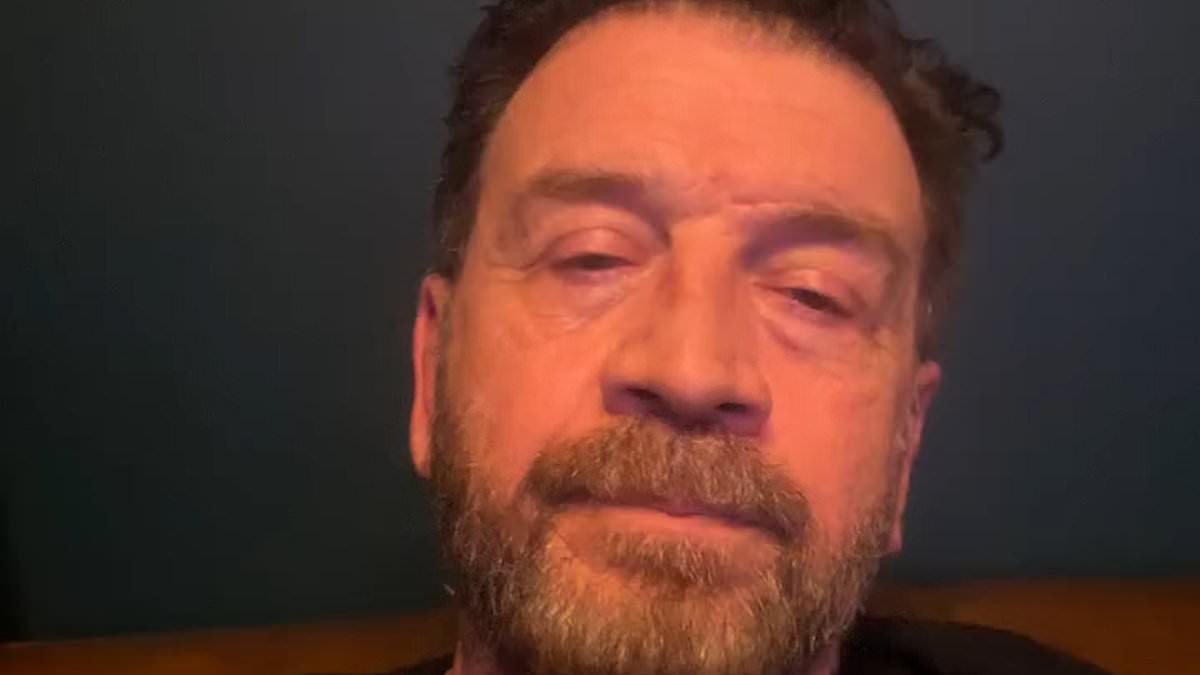
Luigi Mangione, 26, was arrested in Pennsylvania days after the shooting death of UnitedHealthcare CEO Brian Thompson

Chris McNaughton, 33, battled with United for years after the company denied his claims to be treated for a severely debilitating illness that has changed his life forever
Chris McNaughton, 33, battled with United for years after the company denied his claims to be treated for a severely debilitating illness that has changed his life forever.
luHe claimed he was involved in a life-or-death showdown which was dragged out by the company in an effort to save money when the cost of treatment reached nearly $2 million per year.
McNaughton suffers from a crippling case of ulcerative colitis which caused him to develop severe arthritis, extreme bloody diarrhea, brutal fatigue and blood clots that could kill him.
He said that in 2015 he was referred to gastroenterologist at the Mayo Clinic in Minnesota who recommended a high-dose cocktail of medications that successfully reduced his suffering.
‘If you told me in 2015 that I would be living like this, I would have asked where do I sign up,’ he told ProPublica in 2023.
He had been on his parents’ United plan but when he enrolled at Penn State in 2020 he signed on with United’s plan for students in July the same year. In September, United said payments on his claims were ‘pending,’ according to the ProPublica report.
In January, 2021, the company said the outstanding payments for the five months beginning in September were ‘denied’ – and McNaughton was facing a bill of $807,066 which could drag his family into bankruptcy.
According to a lawsuit McNaughton eventually filed, his mother, Janice Light, 70, reached out the next day to ask why the bills which had previously been paid during the summer – but were now being denied – she was told it was because of ‘a high dollar amount on the claims.’
Internally, United had labeled McNaughton’s case a ‘high dollar account’ and they didn’t want to keep paying for the expensive high-dose cocktail of drugs he’d been prescribed.
In August 2021, McNaughton filed a federal lawsuit against United, which wanted to drastically reduce the dosage he received.
During discovery, it emerged that staff had laughed out loud when discussing his case and that the company had been scheming to make sure he would never be approved.
‘On the 2021 phone call, which was recorded by the company, nurse Victoria Kavanaugh told her colleague that a doctor contracted by United to review the case had concluded that McNaughton’s treatment was ‘not medically necessary’. Her colleague, Dave Opperman, reacted to the news with a long laugh,’ ProPublica reported.
Employees also misrepresented critical information to do with his case and ignored warnings from doctors about reducing his dosage.
The ordeal had a huge impact on McNaughton and he considered taking his own life.
At one point a United staffer informed him that the doctor had agreed to lower the dosage of the drugs he was receiving, which was untrue.
‘When we got the denial and they lied about what the doctor said, it just hit me that none of this matters,’ said McNaughton. ‘They will just say or do anything to get rid of me. It delegitimized the entire review process. When I got that denial, I was crushed.’
On May 24, 2021, a new report produced on McNaughton’s case for the Medical Review Institute of America concluded that lowering his dosage ‘can result in a lack of effective therapy for Ulcerative Colitis, with complications of uncontrolled disease (including dysplasia leading to colorectal cancer), flare, hospitalization, need for surgery, and toxic megacolon.’
But, says the lawsuit, United buried the MRIoA report and, instead, denied for a third time McNaughton’s request to stay on a higher dose.
The next month, United agreed to pay for his treatment through the end of the 2012-2022 academic year.
Today, McNaughton is a student at Penn State’s law school and wants to become a health insurance lawyer in order to help other people who have been through the same ordeal as him.
In February last year, lawyers for UnitedHealthcare and McNaughton filed a joint stipulation of dismissal in federal court as part of an agreement to settle the lawsuit.

Jenn Coffey underwent ‘radical’ breast cancer surgery but after the procedure noticed she couldn’t walk properly and developed complex regional pain syndrome

UHC paid just $1.22 towards one payment. When Coffey appealed the amount was reduced down to $1.01. And, thus, she had to file another complaint

When she received the bills for the infusion, the cost wasn’t covered. The company denied all the payments
Jenn Coffey, 53, had spent her whole career working in health care as a nursing assistant, EMT and cardiac technician for 20 years.
‘I carried a pager and would respond to 911 calls in my town as a volunteer,’ she told DailyMail.com.
Then, at the age of 42, Coffey went in for a routine scan and was told she had breast cancer. She underwent ‘radical’ surgery but after the procedure noticed she couldn’t walk properly.
‘My body was a mess,’ recalled Coffey, of Manchester, New Hampshire. ‘My core was destroyed and I was left in a wheelchair.’
She ended up developing complex regional pain syndrome – CRPS – also known as the ‘suicide disease’ because the resulting pain is so unbearable and out of proportion to the original illness.
Explains Coffey: ‘There isn’t a cure. There are treatments, but 70 percent of people who get it, whether they’re young or old will choose suicide.
Having CRPS is like ‘walking around feeling like you’re literally burning on fire, walking on broken glass and barbed wire wrapped around your legs.
‘It is literally torture. People shouldn’t have to suffer but it’s because access to the treatments is so difficult.
‘A doctor told me that he felt that he could save my life if I could just get myself these infusions.’
Five years ago she started a GoFundMe to try and raise enough money to start the monthly infusions which initially cost $5,000.
‘The end result is the symptoms calmed down. It’s as if the infusion acted like a fire hose and simmered down the flame.
‘I could walk around easier or, you know, just be able to cook a meal for myself.’
But the cost of the individual infusions was sky-rocketing up to $600 each time – with Coffey having to pay out of her own pocket. She tried reducing the number of infusions but her health declined.
Coffey posted a video on Twitter (now X) about her predicament and United contacted her.
The company said it would contribute towards the cost of the infusions and so Coffey requested prior authorization which was granted.
But when she received the bills for the infusion the cost wasn’t covered. The company denied all the payments. And so she embarked on a battle with the company and even enrolled the help of her state senators.
‘Getting approval has always been a game,’ said Coffey. ‘And then if you have approval, they still don’t pay. Or they’ll pay just a bit and leave me on the hook for the rest.’
In fact, UHC paid a princely $1.22 towards one payment. When Coffey appealed the amount was actually reduced down to $1.01. And, thus, she had to file another complaint.
‘I have to shop around to find ways to afford the meds that the insurance won’t cover,’ says Coffey. ‘There’s thousands of us (with CPRS) across the country fighting for treatments. In my community, that’s the difference between life and death.’
She added: ‘I wish health insurance companies would stop denying care and start saving more lives. I mean, how much profit do they need?’

Alyssa Bellamy started taking Ozempic to manage her diabetes, but when her doctor tried to increase the dose, UnitedHealthcare refused to cover it

Bellamy said it was scary that her experience was so common among health insurance customers
Alyssa Bellamy was first diagnosed with diabetes in 2022. It had been a rough year for her, dealing with a string of medical complaints.
The 42-year-old Colorado teacher spent the year attempting to change her diet, exercising, and ‘doing as much as I could to get my diabetes under control – my blood sugar level was very high.’
She tried taking Metformin but her kidneys started to fail.
In December 2023, her doctor said she would be a good candidate for Ozempic which she began taking the same month. UnitedHealthcare approved of a dose of 0.5mg, consisting of one injection per week.
She lost 20 lbs by March. But when her doctor wanted to up the dose to 1mg UHC refused the request.
The doctor called the company as well but the repeated requests were still denied. She was told she needed to get another approval for the new dosage.
While Bellamy waited, she rationed out the 0.5mg dose but the small amount had become less effective and her health was being impacted. Weeks passed and she ran out the drug.
‘I didn’t have any medicine, and they wouldn’t give me any more,’ explained Bellamy. ‘We finally got it fixed but I had to go two weeks without any medicine when I got sick, and no one offered any sort of solution.
‘They didn’t care that my doctor had changed the prescription, not me. And they didn’t really care that without my medicine, my blood sugar shoots up so high that it becomes dangerous for me.’
Bellamy contacted People’s Action, an advocacy group, for support.
‘There are a lot of people who deal with diabetes, who don’t have the privilege of being able to get medicine that they need,’ she said.
‘My story isn’t the most terrifying sort of thing that happens, but it’s a very common thing, which is what makes it scary.’
DailyMail.com has contacted UnitedHealthcare for comment.